Appropriate Antibiotic Use
This document was uploaded by user and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this DMCA report form. Report DMCA
Overview
Download & View Appropriate Antibiotic Use as PDF for free.
More details
- Words: 7,487
- Pages: 9
Pediatr Infect Dis J, 2003;22:1143–51 Copyright © 2003 by Lippincott Williams & Wilkins, Inc.
Vol. 22, No. 12 Printed in U.S.A.
Appropriate antibiotic use and why it is important: the challenges of bacterial resistance JAY M. LIEBERMAN, MD
After the introduction of antibiotics in the mid-20th century, clinicians soon witnessed clinical failures secondary to bacterial resistance. Despite scientists’ efforts to synthesize more potent antibiotics during the last five decades, bacterial resistance continues to evolve, in large part because of the overuse and misuse of antibiotics. The treatment of several pathogens, including methicillin-resistant Staphylococcus aureus, penicillin-resistant Streptococcus pneumoniae and vancomycin-resistant enterococci, is problematic. New solutions are needed to preserve the activity of our current antibiotic armamentarium, to lower the overall risk of bacterial resistance and to successfully treat patients with resistant bacterial infections. Options include: development of new antibiotics to treat resistant organisms; vaccination to prevent infections; and improved use of antibiotics. Because bacteria will eventually develop means to avoid being killed by antibiotics, judicious use of antibiotics by all clinicians is imperative. Appropriate antibiotic use involves selection of a “targeted spectrum” antibiotic, as well as an appropriate dose and duration.
priate antibiotic use and a focus on the fluoroquinolones. RESISTANT ORGANISMS
As examples of the clinical challenges posed by bacterial resistance, three Gram-positive organisms are highlighted in this review: Staphylococcus aureus; Streptococcus pneumoniae; and Enterococcus. Methicillin-resistant Staphylococcus aureus. In 1941 all S. aureus organisms were susceptible to penicillin, and relatively low doses of penicillin were highly effective for staphylococcal infections. However, by 1944 S. aureus isolates were described that produced penicillinase,1 an enzyme that inactivates penicillin and renders S. aureus resistant to its effects. By the 1960s most S. aureus isolates were penicillinresistant.2 Because most S. aureus organisms were no longer susceptible to penicillin, new antistaphylococcal drugs were developed, and the semisynthetic penicillins such as methicillin, nafcillin and oxacillin became the mainstays of therapy. However, S. aureus soon developed resistance to these drugs as well. In distinction to penicillin, resistance to the semisynthetic penicillins is not caused by inactivation of the antibiotic but rather is mediated by a change in the target of the antibiotic, an enzyme on the bacterial inner membrane called a penicillin-binding protein. Because the mechanism of resistance is an alteration in the target of the antibiotic, these so-called “methicillin-resistant S. aureus” (MRSA) are resistant clinically to all beta-lactam antibiotics, even though a drug such as cefazolin may appear to be active in vitro. It is also important to note that MRSA are often multidrug-resistant and are resistant to antibiotics such as the macrolides and aminoglycosides, even though the mechanisms of action of these antibiotics are different than that of the betalactams. MRSA became prevalent by the late 1970s, but MRSA infections usually were confined to the large hospital setting. Community-acquired methicillinresistant S. aureus (CA-MRSA) infections were very unusual, particularly in children, until the 1990s, when CA-MRSA emerged in the United States. Chicago Children’s Hospital reported that the number of children hospitalized with CA-MRSA increased from 8
INTRODUCTION
The emergence of antimicrobial resistance among a number of bacterial pathogens changes the way we practice medicine and places some of our patients at risk of dying from their infections. The overuse and misuse of antibiotics are major contributing factors to bacterial resistance; therefore it is incumbent on each of us to use antibiotics appropriately. This article reviews some of the clinical problems we face as a result of bacterial resistance and then discusses potential solutions, with an emphasis on approMiller Children’s Hospital, Long Beach, CA; and University of California, Irvine, CA. Key words: Bacterial resistance, quinupristin/dalfopristin, linezolid, fluoroquinolones. Address for reprints: Jay M. Lieberman, M.D., Miller Children’s Hospital, 2801 Atlantic Avenue, P.O. Box 1428, Long Beach, CA 90801-1428. Fax 562-997-9634; E-mail [email protected].
1143
1144
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
in the 3-year period from 1988 to 1990 to 35 in the 3-year period from 1993 to 1995.3 In south Texas, 53 CA-MRSA infections were identified between 1997 and 2000, compared with just 7 cases between 1990 and 1996.4 The proportion of community-acquired S. aureus infections in children hospitalized at Texas Children’s Hospital in Houston that was methicillinresistant increased from 35% in February 2000 to 67% in January 2002.5 In 1999 the CDC reported 4 pediatric deaths from CA-MRSA in Minnesota and North Dakota.6 The emergence of CA-MRSA as a significant pediatric pathogen in many parts of the US has important clinical implications. Physicians need to know the prevalence of CA-MRSA in their communities and, in areas where CA-MRSA is prevalent, children hospitalized with potentially life-threatening staphylococcal infections, such as endocarditis, should be empirically treated with vancomycin until susceptibilities are available. For non-life-threatening infections, such as lymphadenitis, cellulitis, osteomyelitis or pneumonia in nontoxic patients, clindamycin is usually an appropriate choice.7 Community-acquired MRSA are much more likely to be susceptible to clindamycin than are hospital-acquired MRSA.2– 4 To further complicate matters for clinicians, MRSA that are clindamycin-susceptible but erythromycinresistant may exhibit inducible resistance to clindamycin (i.e. on exposure to clindamycin, such isolates may develop resistance to clindamycin). At the University of Illinois in Chicago, 33 of 88 clindamycin-susceptible MRSA isolates were erythromycin-resistant.8 Evaluation for inducible clindamycin resistance using the “D test” showed that 31 of the 33 isolates exhibited inducible resistance. There was one clinical failure caused by such an isolate; a 9-month-old boy with empyema caused by a clindamycin-susceptible, erythromycinresistant MRSA developed a clindamycin-resistant isolate during clindamycin therapy. Therefore clindamycin should not be prescribed for long term therapy of significant MRSA infections, such as osteomyelitis or empyema, unless the organism is documented to lack inducible resistance to clindamycin. In contrast to the report from Chicago,8 the prevalence of MRSA with inducible clindamycin resistance appears to be lower in other geographic regions.7 Penicillin-resistant Streptococcus pneumoniae. Clinical isolates of S. pneumoniae are reported as susceptible (MIC ⱕ 0.06 g/ml), intermediate (0.12 g/ml ⱕ MIC ⱕ 1 g/ml), or resistant (sometimes referred to as highly resistant; MIC ⱖ 2 g/ml) to penicillin. The clinical significance of these breakpoints is that infections caused by intermediate strains of pneumococcus, with the exception of meningitis, are likely to respond to third generation cephalosporins or even high dose penicillin. Commonly used beta-lactam
Vol. 22, No. 12, Dec. 2003
antibiotics therefore will often be effective for pneumonia, otitis media or sinusitis caused by an intermediate strain of pneumococcus. On the other hand if the pneumococcus is highly resistant, penicillin will not be effective, and these organisms may also be resistant to cefotaxime and ceftriaxone. Penicillin-resistant pneumococci, like CA-MRSA, emerged in the US in the 1990s. In a study of invasive pneumococcal isolates from eight sites around the US in 1998, 24% were nonsusceptible (either intermediate or highly resistant) and 14% overall were highly resistant.9 Similarly a national surveillance study performed in 1999 through 2000 showed that 34% of clinical isolates (invasive and noninvasive) were penicillin-nonsusceptible and 22% overall were highly resistant.10 Resistance had increased markedly compared with a similar study from 1994 through 1995 when 24% of isolates were nonsusceptible and 10% overall were highly resistant.10 As with CA-MRSA the emergence of drug-resistant pneumococci has changed pediatric practice. A child who is hospitalized with a potentially life-threatening pneumococcal infection, such as definite or probable bacterial meningitis, should be treated with an empiric antibiotic regimen that includes vancomycin in addition to cefotaxime or ceftriaxone.11 Importantly vancomycin is not indicated for all children hospitalized with possible or probable pneumococcal infections, such as pneumonia, unless they are critically ill. The treatment for documented resistant invasive pneumococcal infections, such as meningitis, should be based on susceptibility results and may require vancomycin plus another agent such as ceftriaxone or cefotaxime, meropenem and/or rifampin. Some fluoroquinolone antibiotics (e.g. moxifloxacin, gatifloxacin) have excellent activity against penicillin-resistant pneumococci and, although these agents are not yet approved for use in children ⬍18 years of age, they may have a role in the management of serious, resistant pneumococcal infections in children. Consultation with an infectious disease specialist should be strongly considered to assist in the management of invasive pneumococcal infections caused by nonsusceptible organisms. For the more common pneumococcal infections, such as acute otitis media and sinusitis, therapy can be problematic because no oral agent is active against all resistant strains. A consensus statement on otitis media by a CDC working group and clinical practice guidelines for sinusitis from the American Academy of Pediatrics (AAP) provide some recommendations for the management of these infections in an era of pneumococcal resistance.12, 13 Amoxicillin is the drug of choice for uncomplicated acute otitis media or sinusitis regardless of the local prevalence of resistant pneumococci. Even when pneumococci are resistant to penicillin, sufficient concentrations of amoxicillin can often be
Vol. 22, No. 12, Dec. 2003
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
achieved in middle ear and sinus fluid to successfully treat the infection. For children with ear infections who are at increased risk of having a resistant pneumococcal infection (i.e. young infants and those who have recently received antibiotics or who attend day care), high dose amoxicillin (80 to 90 mg/kg/day) is recommended, and many experts recommend high dose amoxicillin for all children with acute otitis media. For children with otitis media who do not respond clinically after 2 to 3 days of amoxicillin therapy, several drugs may be useful as secondary agents, including high dose amoxicillin/clavulanate, cefdinir, cefuroxime axetil, cefpodoxime proxetil or a single intramuscular dose of ceftriaxone. Some data, however, suggest that three once daily doses of ceftriaxone may be required for penicillin-nonsusceptible pneumococcal ear infections.14 It is important to emphasize that some antibiotics commonly used to treat children with ear and sinus infections are unlikely to be effective against nonsusceptible strains of pneumococcus.12 Cefaclor, loracarbef and cefixime, for example, are poorly active against these organisms and therefore should not be used as first line therapy for acute otitis media or sinusitis. It might be thought that other oral antibiotics, such as trimethoprim-sulfamethoxazole and the macrolides, would maintain their activity against penicillinresistant pneumococci because they have a mechanism of action different from that of penicillin. However, as with MRSA, penicillin-resistant pneumococci are usually multidrug-resistant. More than 80% of penicillinresistant pneumococci are also resistant to trimethoprim-sulfamethoxazole and more than one-half are resistant to the macrolides.9 Vancomycin-resistant Enterococcus. Enterococci are normal inhabitants of the human gastrointestinal tract. These bacteria, which are intrinsically resistant to most antimicrobials, including cephalosporins, generally do not cause significant infections in otherwise healthy children. However, enterococci are common causes of hospital-acquired infection, in large part because the widespread use of cephalosporins in hospitalized patients kills most Gram-negative enteric bacteria and leaves enterococci as the predominant organism.15 Therapy of enterococcal infections has become increasingly problematic because of the emergence of resistance. Before 1983 all strains were susceptible to ampicillin, and the recommended therapy for serious enterococcal infections was a synergistic combination of ampicillin and gentamicin. With the emergence of ampicillin resistance, vancomycin became the drug of choice for serious ampicillin-resistant enterococcal infections. In 1986, however, vancomycin-resistant enterococci (VRE) were first reported,16 and rates of isolation of VRE in hospitals increased steadily
1145
through the 1990s.17 From the clinical perspective the emergence of VRE was important because these isolates were often resistant to all available antibiotics, meaning that some patients had untreatable bacterial infections. Vancomycin resistance among enterococci is also important because it is plasmid-mediated. The capacity for vancomycin resistance, therefore, could be transferred in the laboratory to other Gram-positive bacteria. The major concern was the clinical consequence when S. aureus or Streptococcus pneumoniae became vancomycin-resistant. Vancomycin-resistant Staphylococcus aureus. Clinical isolates of MRSA that were intermediate to vancomycin, called vancomycin-intermediate S. aureus (VISA), were first identified in patients in Japan in 199618; as of June 2002, 8 VISA infections had been documented in patients in the US.19 The mechanism of vancomycin resistance among VISA is not the same as it is for VRE. In June 2002 the first clinical isolate of vancomycinresistant S. aureus (VRSA) was reported from a patient in Michigan.19 The patient was a 40-year-old woman with multiple medical problems, including diabetes mellitus, peripheral vascular disease and chronic renal failure. She had recurrent infections of foot ulcers and received multiple courses of broad spectrum antibiotics to treat these infections. In April 2002 the patient developed MRSA bacteremia and was treated with vancomycin. In June 2002 cultures from a suspected catheter exit site infection grew VRSA that contained the vanA gene that confers vancomycin resistance on VRE. A second documented VRSA infection was reported from Pennsylvania in September 2002. This patient also had chronic foot ulcers, and the VRSA isolate contained the vanA resistance gene.20 For these two patients with VRSA infection, there were other therapeutic options, but the threat of untreatable S. aureus infections looms closer on the horizon. It seems only a matter of time before children develop common infections, such as staphylococcal cellulitis or lymphadenitis, that are resistant to all routinely used oral antibiotics. Why bacterial resistance? Microbes have genetic plasticity, which means that they have the capacity to evolve in response to their environment. The major impetus for developing resistance is selective pressure resulting from antibiotic use. The bacteria that survive are those that develop mechanisms to avoid being killed by antibiotics. What is this antibiotic pressure? In the United States, an estimated 126 million courses of antibiotics were prescribed in the ambulatory setting in 2000.21 Pediatricians have a special responsibility for controlling this problem because children account for a disproportionate share of the antibiotics used. Ear infec-
1146
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
tions alone resulted in almost 30 million office visits in 1997. With all this selective pressure from antibiotic use, bacterial resistance emerges. Because of bacterial resistance, patients present with more serious infections or with infections that are more difficult to treat. This leads to more antibiotic use and the use of more broad spectrum agents. And so a vicious cycle develops. For example it is necessary to limit vancomycin use because of VRE and concerns about the emergence of vancomycin resistance among staphylococci and streptococci. However, because of the increasing prevalence of MRSA and drug-resistant pneumococci, we use more vancomycin. The place to break this vicious cycle is to decrease antibiotic use and thereby decrease the pressure on bacteria to develop resistance. Three major approaches are advocated to combat bacterial resistance: (1) develop new antibiotics to treat resistant organisms; (2) vaccinate to prevent infections; and (3) improve our use of antibiotics. NEW ANTIBIOTICS
Quinupristin/dalfopristin. Quinupristin/dalfopristin (Synercid) is a semisynthetic antibiotic that combines two streptogramin compounds and is the first licensed antibiotic in its class.22 It inhibits bacterial protein synthesis and is available only as an intravenous product. Its spectrum of activity is similar to that of vancomycin, with excellent activity against Grampositive pathogens, including many resistant strains. Quinupristin/dalfopristin is active against staphylococci, including MRSA, pneumococci, including penicillin-resistant strains, and Enterococcus faecium, including VRE (but not Enterococcus faecalis). Its major value is that it provides a therapeutic option for infections caused by vancomycin-resistant E. faecium, VISA or VRSA. In addition quinupristin/dalfopristin may be useful for treatment of serious Gram-positive infections in patients who are allergic to, or intolerant of, beta-lactams and vancomycin. Unfortunately there are already reports of VRE and MRSA resistant to quinupristin/dalfopristin since its licensure in 1999.23, 24 Linezolid. Linezolid (Zyvox) is the first licensed oxazolidinone antibiotic.25 The oxazolidinones, synthetic compounds unrelated to other antimicrobials, inhibit bacterial protein synthesis. Linezolid has limited activity against selected Gram-negatives and anaerobes but is highly active against Gram-positive bacteria, including resistant strains. Like quinupristin/dalfopristin, linezolid is active against MRSA, penicillin-resistant pneumococci and vancomycin-resistant E. faecium. Unlike quinupristin/dalfopristin, linezolid also is active against E. faecalis. Linezolid is available in both intravenous and oral preparations and is 100% bioavailable after oral administration. As such it provides an oral therapeutic
Vol. 22, No. 12, Dec. 2003
option for patients with Gram-positive infections resistant to other oral antibiotics. Therapy with linezolid should be limited to patients with infections caused by VRE, VISA or VRSA; for serious Gram-positive infections in patients who cannot tolerate vancomycin or beta-lactam antibiotics; and for patients with resistant Gram-positive infections who have been treated with intravenous vancomycin and can be transitioned to oral therapy. Since linezolid became available in 2000, clinical isolates of VRE and MRSA resistant to linezolid have been reported from treated patients.26 –28 Quinupristin/dalfopristin and linezolid are two valuable additions to our antimicrobial armamentarium, but resistance has already been described. To preserve their value their use should be limited to those rare cases where they are clearly needed. Fluoroquinolones. Although the fluoroquinolones are not new antibiotics, most pediatricians have limited experience with this class of antibiotics. Important features of this drug class include excellent bioavailability after oral administration, achievement of high tissue concentrations and a broad spectrum of activity. In general fluoroquinolones are active against many Gram-positive bacteria (the “newer” quinolones, moxifloxacin and gatifloxacin, are particularly active against Streptococcus pneumoniae) and many Gramnegative bacteria. Some quinolones (ciprofloxacin being the most potent) have significant activity against Pseudomonas aeruginosa.29 The quinolones are therefore attractive agents to use for treatment of selected children with serious bacterial infections. The quinolones have a unique mechanism of action; they inhibit two bacterial enzymes, DNA gyrase and topoisomerase IV, that are essential for bacterial DNA synthesis. Because they target bacterial sites distinct from the site of action of other antibiotics, it was hypothesized by some that resistance might be less likely to occur or slower to develop.30 Unfortunately these hopes were not borne out. Oral ciprofloxacin first became available in the US in October 1987 and rapidly became a widely prescribed antibiotic. By 1989 it was the fourth most prescribed antibiotic in the country, with ⬎5 million prescriptions filled.31 During the last decade a number of other fluoroquinolones have become available, including ofloxacin, levofloxacin, moxifloxacin and gatifloxacin. With widespread use during the past 15 years, quinolone resistance has emerged among a number of bacteria. Four such organisms are highlighted here. Neisseria gonorrhoeae. Fluoroquinolone antibiotics, such as ciprofloxacin, ofloxacin and levofloxacin, given as a single oral dose are among the recommended therapies for uncomplicated gonorrhea. However, N. gonorrhoeae isolates resistant to the quinolones emerged in the 1990s and are now prevalent in parts of Asia and the Pacific. Such isolates have been identified
Vol. 22, No. 12, Dec. 2003
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
only sporadically throughout the US, although in Hawaii the percentage of isolates that are ciprofloxacinresistant increased from 1.4% in 1997 to 14.3% in 2000.32, 33 As a result, before treating a patient with gonorrhea, a travel history should be obtained from both the patient and their sexual partner(s). If either is likely to have acquired the infection in Asia, the Pacific Islands or Hawaii, then a quinolone should not be used. Because of an increased prevalence of quinolone resistance among N. gonorrhoeae isolates in California, the CDC has also stated that the use of fluoroquinolones in that state “is probably inadvisable.”33 S. pneumoniae. The newer quinolones (e.g. moxifloxacin, gatifloxacin) are now among the recommended agents for the empiric treatment of community-acquired pneumonia in adults. 34 In Canada prescriptions for quinolones in general increased almost 7-fold between 1988 and 1998 (from 0.8 to 5.5 prescriptions per 100 persons per year).35 Through 1993 pneumococci with reduced susceptibility to the quinolones had not been identified but, by 1997 through 1998, the prevalence of S. pneumoniae strains nonsusceptible to ciprofloxacin isolated from Canadian adult patients had increased to 2.9%. All strains isolated from children were susceptible. Furthermore patients with pneumococcal pneumonia who failed empiric levofloxacin therapy because of infections with levofloxacin-resistant strains (including patients whose isolates developed resistance during therapy) have been reported.36, 37 Although the overall prevalence of quinolone-resistant pneumococci remains relatively low, it is interesting to recognize that penicillin was available for almost 50 years before clinically significant penicillin resistance emerged. It took fewer than 10 years for quinolone resistance to develop among the pneumococci. Campylobacter/Salmonella. The quinolones are widely prescribed for the treatment of patients with bacterial gastroenteritis because this class of drugs is active against a broad range of bacterial pathogens that cause diarrhea, including Salmonella, Shigella, Campylobacter and Yersinia. In Minnesota, however, the proportion of Campylobacter jejuni resistant to the quinolones increased from 1.3% in 1992 to 10.2% in 1998.38 Many of these cases were associated with foreign travel and recent quinolone use. This phenomenon is not limited to Minnesota; 40.5% of C. jejuni isolates were fluoroquinolone-resistant in one Pennsylvania health care system in 2001.39 Fluoroquinolone resistance also has emerged among Salmonella species. In Taiwan, ciprofloxacin resistance was not seen among Salmonella enterica serotype choleraesuis until 2000. By the third quarter of 2001, 60% of isolates in Taiwan were ciprofloxacin-resistant.40 An analysis of S. enterica isolates from Finnish travelers also showed that the proportion with reduced suscep-
1147
tibility to ciprofloxacin increased from 3.9% in 1995 to 23.5% in 1999.41 One reason quinolone resistance has emerged among enteric bacteria is that, in some regions of the world, these antibiotics are used in livestock and poultry not only to treat infections in the animals but, more importantly, to promote growth after administration of subtherapeutic concentrations.42 This long term exposure to low levels of antibiotics provides an ideal environment for the selection of resistant bacteria in the animals. Although quinolones are not approved for growth promotion, they are known to be misused, especially outside the US.43 In the US quinolone antibiotics were approved for therapeutic use in poultry in 1995. In Minnesota C. jejuni was isolated from 74% of 91 retail chicken products in 1997, and 14% of these isolates were ciprofloxacin-resistant.38 Many public health experts want to prohibit the use of antibiotics in poultry, especially those antibiotics that are used to treat infections in humans.44 In 1999 the European Union banned the use of four such antibiotics as growth promoters.45 The US Food and Drug Administration may soon follow suit. The experience with the quinolones exemplifies the lesson that inappropriate use of an antibiotic hastens the development of resistance. The more an antibiotic is used, the more pressure there is on bacteria to develop resistance. If antibiotics are not used judiciously, they can lose their value and thus not be available for patients who really need them. Appropriate use of fluoroquinolones in children. Although the quinolones are not currently approved for use in patients younger than 18 years of age, they already have an established role in certain high risk pediatric populations. They are commonly used to treat pulmonary exacerbations caused by P. aeruginosa in children who have cystic fibrosis and may also have a role in the prevention or treatment of infections in children with cancer. Several potentially appropriate uses for quinolones in otherwise healthy children are listed in Table 1.
TABLE 1. Possible uses for fluoroquinolone antibiotics in otherwise healthy children* Infections caused by Pseudomonas aeruginosa or other multidrug-resistant Gram-negative bacteria Urinary tract infection Chronic suppurative otitis media or malignant otitis externa Chronic osteomyelitis Complicated middle ear and mastoid infections Bacterial gastroenteritis caused by a multidrug-resistant organism, e.g. Shigella Typhoid fever Mycobacterial infections Anthrax prophylaxis or treatment * Fluoroquinolone antibiotics are not licensed for use in individuals younger than 18 years of age, except in the case of anthrax treatment. If use is recommended for a patient younger than 18 years of age, the risks and benefits should be explained to the patient, when appropriate, and parents.
1148
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
They should not be used to treat children with colds or bronchitis or for children who have infections susceptible to other oral antibiotics. In general the quinolones should be reserved for treating specific bacterial infections (e.g. P. aeruginosa) that are resistant to commonly used antibiotics or when the use of an oral quinolone allows outpatient management of a serious infection for which no other oral agent is available. IMMUNIZATIONS
New antibiotics will never completely solve the bacterial resistance problem because organisms eventually develop resistance. New vaccines, on the other hand, may provide a solution. By the 1970s a significant proportion of Haemophilus influenzae type b (Hib) isolates was resistant to ampicillin and chloramphenicol. It seemed inevitable that Hib would develop resistance to ceftriaxone and cefotaxime. However, antibiotic-resistant Hib meningitis is no longer of concern because widespread use of the Hib conjugate vaccines has eliminated the disease. Similarly concerns about treating resistant pneumococcal infections can be alleviated through use of the pneumococcal conjugate vaccine. Vaccination against viral diseases also can reduce antibiotic use. Preventing chickenpox through use of the varicella vaccine can avert secondary bacterial infections caused by S. aureus and eliminate concerns about possible MRSA infection. Preventing influenza may thwart secondary bacterial ear infections and pneumonia. In a study of a nasal spray influenza vaccine in children, vaccinated children had 21% fewer febrile illnesses and 30% fewer episodes of febrile otitis media than did unvaccinated controls.46 Widespread vaccination against influenza among young children, as encouraged by the current recommendations,47 will lead to fewer fevers and fewer antibiotic prescriptions. Decreasing antibiotic use can reduce the emergence of resistance. IMPROVING ANTIBIOTIC USE
Judicious antibiotic use means that antibiotics are prescribed only when indicated and that the drug chosen is the most narrow spectrum agent that will be effective. Appropriate use means choosing not only the correct antibiotic but also the appropriate dose and duration, factors that can influence the development and carriage of resistant organisms.29, 48 In an observational study of children in France, the use of an oral beta-lactam agent was associated with an increased risk of pharyngeal carriage of penicillinresistant Streptococcus pneumoniae. The risk was highest in those children who had been prescribed a lower than recommended dose of the antibiotic and in those who had received ⬎5 days of therapy.49 A randomized trial conducted in Chile confirmed these find-
Vol. 22, No. 12, Dec. 2003
ings. The rate of carriage of penicillin-nonsusceptible pneumococci was significantly lower in children prescribed amoxicillin at 90 mg/kg/day for 5 days compared with children prescribed 40 mg/kg/day for 10 days.50 Understanding that low dose and/or prolonged antibiotic usage selects for bacterial resistance can lead to beneficial changes in physicians’ antibiotic prescribing practices.51 The results of a metaanalysis suggest that 5 days of antibiotic therapy is effective for uncomplicated acute otitis media,52 and short course therapy is recommended for children 2 years of age and older with uncomplicated ear infections.11 Clinical research may define other pediatric infections for which a shorter course of antibiotics is appropriate. The importance of appropriate antibiotic use is magnified by the fact that these drugs have an impact on the community as well as on the child for whom they are prescribed. An antibiotic alters a child’s microbial flora and, for example, increases the likelihood that the child will be colonized with a penicillin-resistant pneumococcus. Although that child may never develop pneumococcal disease, children in the same day-care center or a younger sibling may acquire that resistant organism and develop an ear infection or meningitis. After an 11-month-old child in a Georgia day-care center developed refractory otitis media caused by a multidrug-resistant pneumococcus, other children in the center were evaluated for nasal carriage of the organism. Of 21 children tested 10 (48%) carried the same highly resistant pneumococcus.53 Similarly a child in an intensive care unit who is treated with extended spectrum cephalosporins may become colonized with resistant pathogens such as VRE or multidrug-resistant Gram-negative bacteria. These highly resistant pathogens can then be transmitted via the hands of a health care worker to a child in a neighboring bed who may develop a serious infection. The implication is that every time an antibiotic is prescribed, there is a multiplier effect. Every antibiotic given to a child may adversely affect 2 or 5 or 10 children. However, this fact also empowers prescribers, because it means that for every antibiotic not prescribed, 2 or 5 or 10 children are protected from the potential adverse consequences. The good news is that bacterial resistance is to some degree reversible. In response to an increase in erythromycin resistance among group A streptococci in Finland, nationwide recommendations were issued to reduce the use of macrolide antibiotics. As a result macrolide consumption declined by ⬃40%, and the frequency of erythromycin resistance among group A streptococcal isolates subsequently declined by almost one-half.54 Reducing antibiotic use should be effective, because resistant bacteria have no competitive advantage in
Vol. 22, No. 12, Dec. 2003
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
the absence of antibiotic exposure and because colonization with resistant pathogens is usually transient. A study of nasopharyngeal carriage of penicillinresistant pneumococci revealed that cultures were negative within 4 weeks in 68% of carriers, within 8 weeks in 87% and within 12 weeks in 94%.55 Because carriage of these resistant bacteria resolves spontaneously, susceptible strains eventually replace resistant strains in the absence of antibiotic exposure. Antibiotic restrictions do not guarantee that antimicrobial resistance will disappear, however, as demonstrated by a report from the UK.56 Despite a marked decrease in prescriptions for sulfonamides, the frequency of sulfonamide-resistant Escherichia coli did not decrease during an 8-year time period. The reasons for this are not clear, although it may be because the determinants of sulfonamide resistance are genetically linked to other resistance determinants. The AAP and CDC have published principles of judicious antibiotic use for upper respiratory tract infections.57 Key features of these recommendations are highlighted in Table 2. Despite the guidelines inappropriate antibiotic use is common. One report evaluated 531 pediatric office visits in which the discharge diagnosis was cold, upper respiratory tract infection, or bronchitis and found that antibiotics were prescribed for 44% of children with colds, 46% with upper respiratory tract infections and 75% with bronchitis.58 None of these patients required antibiotics, and yet these 3 diagnoses accounted for ⬎20% of all antibiotic prescriptions. In another study physicians were polled regarding
their antibiotic prescribing practices, and 38% of the pediatricians and 58% of the family physicians indicated that they routinely prescribed antibiotics for the common cold.59 In addition 81% of the pediatricians and 93% of the family physicians routinely prescribed antibiotics for bronchitis. A review of their office charts showed that these reported practices correlated with actual practices, given that antibiotics were prescribed for 31% of visits where the common cold was diagnosed. In addition antibiotics were prescribed for 19% of phone encounters and 49% of office visits, including 11% of well-child checkups. There was enormous variability among practitioners, with rates of antibiotic prescribing ranging from 1 to 10 prescriptions per child per year. Pediatricians acknowledge that they sometimes prescribe antibiotics for inappropriate indications60; their reasons for this are multifactorial. Parental pressure is a major factor cited by some clinicians. Parents often desire a tangible product at the conclusion of a visit, and the clinician may feel that they need to satisfy this demand. It is clear that any educational campaign to reduce inappropriate antibiotic use in children must target parents as well as clinicians. Other factors that can influence prescribing practices include concerns about legal liability, economic pressures to evaluate and examine patients quickly and incorrect perceptions about the effectiveness of antibiotics for certain infections.60, 61 Changing physician (and parental) behavior is complex and will require a multifaceted approach, but there is some evidence to suggest this can be accom-
TABLE 2. Principles of judicious use of antimicrobial agents for upper respiratory tract infections* Disease
Principles
Otitis media
1. Antimicrobials are indicated for the treatment of AOM, but the diagnosis requires documented middle ear effusion and signs or symptoms of acute local or systemic illness. 2. A narrow spectrum antibiotic (e.g. amoxicillin) should be used for initial episodes of AOM. 3. Antimicrobials are not indicated for initial treatment of otitis media with effusion, although treatment may be indicated if effusions persist for ⱖ3 mo. 4. Antimicrobial prophylaxis should be reserved for control of recurrent AOM, defined as ⱖ3 distinct and well-documented episodes in 6 mo or ⱖ4 episodes in 12 mo.
Acute sinusitis
1. Clinical diagnosis of bacterial sinusitis requires: nasal discharge and daytime cough without improvement for 10 to 14 days; or more severe signs and symptoms (i.e. fever ⱖ39°C, facial swelling, facial pain). 2. Initial antimicrobial treatment of acute sinusitis should be with the most narrow spectrum agent that is active against the likely pathogens.
Cough illness/bronchitis
1. Nonspecific cough illness/bronchitis in children, regardless of duration, does not warrant antimicrobial treatment.
Pharyngitis
1. Diagnosis of group A streptococcal pharyngitis should be made based on results of appropriate laboratory tests in conjunction with clinical and epidemiologic findings. 2. Antimicrobial therapy should not be given to a child with pharyngitis in the absence of documented group A streptococcal infection. Other rare causes of bacterial pharyngitis, e.g. diphtheria, may require therapy. 3. Penicillin remains the drug of choice for treating group A streptococcal pharyngitis.
Common cold
1. Antimicrobial agents should not be given for the common cold. 2. Mucopurulent rhinitis (thick, opaque or discolored nasal discharge) frequently accompanies the common cold and is not an indication for antimicrobial treatment unless it persists for 10 –14 days suggesting possible sinusitis.
* Adapted from Reference 57, with permission.
1149
1150
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
plished. One study evaluated an educational intervention for pediatricians and family physicians.62 Principles of judicious antibiotic use were discussed with the physicians twice over a 4-month period, and parents were mailed a brochure on antibiotic use. Antibiotic prescribing practices before and after the intervention were compared, as they were in “control” practices in which no intervention was done. In children 3 to 36 months of age, antibiotic dispensing decreased 18.6% in the intervention group vs. 11.4% in the control practices. In another study a community-based intervention trial targeted parents and pediatric primary care providers for education regarding judicious antibiotic use.63 The median number of prescriptions for liquid antibiotics per clinician declined 11% in the intervention region, whereas it increased 12% in the control region. The median number of solid antibiotic prescriptions (tablets and capsules) declined by 19% and 8% in the intervention and control regions, respectively. The results of these two studies should be interpreted with some caution because of baseline differences in antibiotic prescribing rates between the intervention and control groups. Nonetheless they support the idea that educating physicians and parents can positively impact antibiotic use. It is interesting that antibiotic use decreased not only in the intervention groups and regions, but also in many of the control practices and regions. This is a nationwide trend. From 1989 to 1990 through 1999 to 2000, overall antibiotic prescription rates (per patient visit) by office-based physicians in the US declined by 29% for children younger than 15 years of age.64 For children younger than 5 years, the group with the highest antibiotic use, antibiotic prescribing dropped by 41% between 1995 and 1999.65 The message that we need to improve our antibiotic prescribing seems to have been heard. Each of us must do what we can to ensure that this trend continues, because our reward will be less bacterial resistance and healthier children. CONCLUSIONS
Bacterial resistance threatens our ability to treat both common and serious infections in children. Although new antibiotics can effectively treat some resistant pathogens and more research is needed to develop novel antimicrobials, bacteria will eventually develop resistance to any antibiotic with time. The misuse and overuse of antibiotics drive the emergence and spread of resistance. Eliminating inappropriate antibiotic use and promoting more judicious use are essential parts of the solution. REFERENCES 1. Neu HC. The crisis in antibiotic resistance. Science 1992;257: 1064 –73. 2. Chambers HF. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis 2001;7:178 – 82.
Vol. 22, No. 12, Dec. 2003
3. Herold BC, Immergluck LC, Maranan MC, et al. Communityacquired methicillin-resistant Staphylococcus aureus infections in children with no predisposing risk. JAMA 1998;279: 593– 8. 4. Fergie JE, Purcell K. Community-acquired methicillinresistant Staphylococcus aureus infections in south Texas children. Pediatr Infect Dis J 2001;20:860 –3. 5. Sattler CA, Mason EO Jr, Kaplan SL. Prospective comparison of risk factors and demographic and clinical characteristics of community-acquired, methicillin-resistant versus methicillin-susceptible Staphylococcus aureus infection in children. Pediatr Infect Dis J 2002;21:910 –7. 6. Centers for Disease Control and Prevention. Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus: Minnesota and North Dakota, 1997– 1999. MMWR 1999;48:707–10. 7. Martinez-Aguilar G, Hammerman W, Mason EO Jr, Kaplan SL. Clindamycin treatment of invasive infections caused by community-acquired, methicillin-resistant and methicillinsusceptible Staphylococcus aureus in children. Pediatr Infect Dis J 2003;22:593– 8. 8. Frank AL, Marcinak JF, Mangat PD, et al. Clindamycin treatment of methicillin-resistant Staphylococcus aureus infections in children. Pediatr Infect Dis J 2002;21:530 – 4. 9. Whitney CG, Farley MM, Hadler J, et al. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med 2000;343:1917–24. 10. Doern GV, Heilmann KP, Huynh HK, Rhomberg PR, Coffman SL, Brueggemann AB. Antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in the United States during 1999 –2000, including a comparison of resistance rates since 1994 –1995. Antimicrob Agents Chemother 2001;45:1721–9. 11. American Academy of Pediatrics. Pneumococcal infections. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003:490 –500. 12. Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance: a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working Group. Pediatr Infect Dis 1999;18:1–9. 13. American Academy of Pediatrics, Subcommittee on management of sinusitis and committee on quality improvement. Clinical practice guideline: management of sinusitis. Pediatrics 2001;108:798 – 808. 14. Leibovitz E, Piglansky L, Raiz S, Press J, Leiberman A, Dagan R. Bacteriologic and clinical efficacy of one day vs. three day intramuscular ceftriaxone for treatment of nonresponsive acute otitis media in children. Pediatr Infect Dis J 2000;19:1040 –5. 15. Rice LB. Emergence of vancomycin-resistant enterococci. Emerg Infect Dis 2001;7:183–7. 16. Uttley AH, Collins CH, Naidoo J, George RC. Vancomycinresistant enterococci. Lancet 1988;1:57– 8. 17. Murray BE. Vancomycin-resistant enterococcal infections. N Engl J Med 2000;342:710 –21. 18. Smith TL, Pearson ML, Wilcox KR, et al. Emergence of vancomycin resistance in Staphylococcus aureus. N Engl J Med 1999;340:493–501. 19. Chang S, Sievert DM, Hageman JC, et al. Infection with vancomycin-resistant Staphylococcus aureus containing the vanA resistance gene. N Engl J Med 2003;348:1342–7. 20. Centers for Disease Control and Prevention. Vancomycinresistant Staphylococcus aureus: Pennsylvania, 2002. MMWR 2002;51:902. 21. McCaig LF, Besser RE, Hughes JM. Antimicrobial drug prescriptions in ambulatory care settings, United States, 1992–2000. Emerg Infect Dis 2003;9:432–7. 22. Harrison CJ. Quinupristin/dalfopristin. Semin Pediatr Infect Dis 2001;12:200 –10. 23. Dowzicky M, Talbot GH, Feger C, Prokocimer P, Etienne J, Leclercq R. Characterization of isolates associated with emerging resistance to quinupristin/dalfopristin (Synercid®)
Vol. 22, No. 12, Dec. 2003
24.
25. 26. 27. 28.
29. 30. 31. 32.
33. 34.
35.
36. 37.
38. 39. 40. 41.
42. 43.
44.
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
during a worldwide clinical program. Diagn Microb Infect Dis 2000;37:57– 62. Rose CM, Reilly KJ, Haith LR, et al. Emergence of resistance of vancomycin-resistant Enterococcus faecium in a thermal injury patient treated with quinupristin-dalfopristin and cultured epithelial autografts for wound closure. Burns 2002; 28:696 – 8. Diekema DJ, Jones RN. Oxazolidinone antibiotics. Lancet 2001;358:1975– 82. Herrero IA, Issa NC, Patel R. Nosocomial spread of linezolidresistant, vancomycin-resistant Enterococcus faecium. N Engl J Med 2002;346:867–9. Tsiodras S, Gold HS, Sakoulas G, et al. Linezolid resistance in a clinical isolate of Staphylococcus aureus. Lancet 2001; 358:207– 8. Pai MP, Rodvold KA, Schreckenberger PC, Gonzales RD, Petrolatti JM, Quinn JP. Risk factors associated with the development of infection with linezolid- and vancomycinresistant Enterococcus faecium. Clin Infect Dis 2002;35: 1269 –72. Scheld WM. Maintaining fluoroquinolone class efficacy: review of influencing factors. Emerg Infect Dis 2003;9:1–9. Kayser FH. The quinolones: mode of action and mechanism of resistance. Res Clinic Forums 1985;7:17–27. Frieden TR, Mangi RJ. Inappropriate use of oral ciprofloxacin. JAMA 1990;264:1438 – 40. Centers for Disease Control and Prevention. Fluoroquinolone-resistance in Neisseria gonorrhoeae, Hawaii, 1999, and decreased susceptibility to azithromycin in N. gonorrhoeae, Missouri, 1999. MMWR 2000;49:833–7. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines. MMWR 2002;51(RR6):36 – 42. Bartlett JG, Dowell SF, Mandell LA, File TM Jr, Musher DM, Fine MJ. Practice guidelines for the management of community-acquired pneumonia in adults. Clin Infect Dis 2000;31: 347– 82. Chen DK, McGeer A, de Azavedo JC, Low DE. Decreased susceptibility of Streptococcus pneumoniae to fluoroquinolones in Canada: Canadian Bacterial Surveillance Network. N Engl J Med 1999;341:233–9. Davidson R, Cavalcanti R, Brunton JL, et al. Resistance to levofloxacin and failure of treatment of pneumococcal pneumonia. N Engl J Med 2002;346:747–50. Kays MB, Smith DW, Wack ME, Denys GA. Levofloxacin treatment failure in a patient with fluoroquinolone-resistant Streptococcus pneumoniae pneumonia. Pharmacotherapy 2002;22:395–9. Smith KE, Besser JM, Hedberg CW, et al. Quinoloneresistant Campylobacter jejuni infections in Minnesota, 1992–1998. N Engl J Med 1999;340:1525–32. Nachamkin I, Ung H, Li M. Increasing fluoroquinolone resistance in Campylobacter jejuni, Pennsylvania, USA, 1982– 2001. Emerg Infect Dis 2002;8:1501–3. Chiu CH, Wu TL, Su LH, et al. The emergence in Taiwan of fluoroquinolone resistance in Salmonella enterica serotype choleraesuis. N Engl J Med 2002;346:413–9. Hakanen A, Koitlainen P, Huovinen P, Helenius H, Siitonen A. Reduced fluoroquinolone susceptibility in Salmonella enterica serotypes in travelers returning from Southeast Asia. Emerg Infect Dis 2001;7:996 –1003. Tollefson L, Miller MA. Antibiotic use in food animals: controlling the human health impact. J AOAC Int 2000;83: 245–54. Velazquez JB, Jimenez A, Chomon B, Villa TG. Incidence and transmission of antibiotic resistance in Campylobacter jejuni and Campylobacter coli. J Antimicrob Chemother 1995;35: 173– 8. Center for Science in the Public Interest. Protecting the crown jewels of medicine: a strategic plan to preserve the effectiveness of antibiotics. Washington, DC, 1998. [Center for Science in the Public Interest web site]. Available at http://www.cspinet.org/reports/abiotic.htm. Accessed August 27, 2003.
1151
45. Department of Health and Human Services, Food and Drug Administration. HHS response to House Report 106-157: Agriculture, Rural Development, Food and Drug Administration, and Related Agencies, appropriations bill, 2000. Human-use antibiotics in livestock production. [Center for Veterinary Medicine web site]. Available at http://www.fda.gov/ cvm/antimicrobial/HRESP106_157.htm#execsummary. Accessed August 28, 2003. 46. Belshe RB, Mendelman PM, Treanor J, et al. The efficacy of live attenuated, cold-adapted, trivalent, intranasal influenzavirus vaccine in children. N Engl J Med 1998;338:1405–12. 47. Centers for Disease Control and Prevention. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2003;52 (RR-8):7–10. 48. Craig WA. Does the dose matter? Clin Infect Dis 2001; 33(Suppl 3):S233–7. 49. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of beta-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA 1998; 279:365–70. 50. Schrag SJ, Pen˜ a C, Ferna´ ndez J, et al. Effect of short-course, high-dose amoxicillin therapy on resistant pneumococcal carriage: a randomized trial. JAMA 2001;286:49 –56. 51. Levy SB. Antibiotic resistance: consequences of inaction. Clin Infect Dis 2001;33(Suppl 3):S124 –9. 52. Kozyrskyj AL, Hildes-Ripstein GE, Longstaffe SE, et al. Treatment of acute otitis media with a shortened course of antibiotics: a meta-analysis. JAMA 1998;279:1736 – 42. 53. Centers for Disease Control and Prevention. Multidrugresistant Streptococcus pneumoniae in a child care center: southwest Georgia, December 2000. MMWR 2002;50:1156– 8. 54. Seppala H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. N Engl J Med 1997;337:441– 6. 55. Ekdahl K, Ahlinder I, Hansson HB, et al. Duration of nasopharyngeal carriage of penicillin-resistant Streptococcus pneumoniae: experiences from the South Swedish Pneumococcal Intervention Project. Clin Infect Dis 1997;25:1113–7. 56. Enne VI, Livermore DM, Stephens P, Hall LM. Persistence of sulphonamide resistance in Escherichia coli in the UK despite national prescribing restriction. Lancet 2001;357:1325– 8. 57. American Academy of Pediatrics. Appropriate use of antimicrobial agents. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics, 2003:695–7. 58. Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 1998;279:875–7. 59. Watson RL, Dowell SF, Jayaraman M, Keyserling H, Kolczak M, Schwartz B. Antimicrobial use for pediatric upper respiratory infections: reported practice, actual practice, and parent beliefs. Pediatrics 1999;104:1251–7. 60. Bauchner H, Pelton SI, Klein JO. Parents, physicians, and antibiotic use. Pediatrics 1999;103:395– 401. 61. Avorn J, Solomon DH. Cultural and economic factors that (mis)shape antibiotic use: the nonpharmacologic basis of therapeutics. Ann Intern Med 2000;133:128 –35. 62. Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics 2001;108:1–7. 63. Belongia EA, Sullivan BJ, Chyou PH, Madagame E, Red KD, Schwartz B. A community intervention trial to promote judicious antibiotic use and reduce penicillin-resistant Streptococcus pneumoniae carriage in children. Pediatrics 2001; 108:575– 83. 64. McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA 2002; 287:3096 –102. 65. Halasa NB, Griffin MR, Zhu Y, Edwards KM. Decreased number of antibiotic prescriptions in office-based settings from 1993 to 1999 in children less than five years of age. Pediatr Infect Dis J 2002;21:1023– 8.
Vol. 22, No. 12 Printed in U.S.A.
Appropriate antibiotic use and why it is important: the challenges of bacterial resistance JAY M. LIEBERMAN, MD
After the introduction of antibiotics in the mid-20th century, clinicians soon witnessed clinical failures secondary to bacterial resistance. Despite scientists’ efforts to synthesize more potent antibiotics during the last five decades, bacterial resistance continues to evolve, in large part because of the overuse and misuse of antibiotics. The treatment of several pathogens, including methicillin-resistant Staphylococcus aureus, penicillin-resistant Streptococcus pneumoniae and vancomycin-resistant enterococci, is problematic. New solutions are needed to preserve the activity of our current antibiotic armamentarium, to lower the overall risk of bacterial resistance and to successfully treat patients with resistant bacterial infections. Options include: development of new antibiotics to treat resistant organisms; vaccination to prevent infections; and improved use of antibiotics. Because bacteria will eventually develop means to avoid being killed by antibiotics, judicious use of antibiotics by all clinicians is imperative. Appropriate antibiotic use involves selection of a “targeted spectrum” antibiotic, as well as an appropriate dose and duration.
priate antibiotic use and a focus on the fluoroquinolones. RESISTANT ORGANISMS
As examples of the clinical challenges posed by bacterial resistance, three Gram-positive organisms are highlighted in this review: Staphylococcus aureus; Streptococcus pneumoniae; and Enterococcus. Methicillin-resistant Staphylococcus aureus. In 1941 all S. aureus organisms were susceptible to penicillin, and relatively low doses of penicillin were highly effective for staphylococcal infections. However, by 1944 S. aureus isolates were described that produced penicillinase,1 an enzyme that inactivates penicillin and renders S. aureus resistant to its effects. By the 1960s most S. aureus isolates were penicillinresistant.2 Because most S. aureus organisms were no longer susceptible to penicillin, new antistaphylococcal drugs were developed, and the semisynthetic penicillins such as methicillin, nafcillin and oxacillin became the mainstays of therapy. However, S. aureus soon developed resistance to these drugs as well. In distinction to penicillin, resistance to the semisynthetic penicillins is not caused by inactivation of the antibiotic but rather is mediated by a change in the target of the antibiotic, an enzyme on the bacterial inner membrane called a penicillin-binding protein. Because the mechanism of resistance is an alteration in the target of the antibiotic, these so-called “methicillin-resistant S. aureus” (MRSA) are resistant clinically to all beta-lactam antibiotics, even though a drug such as cefazolin may appear to be active in vitro. It is also important to note that MRSA are often multidrug-resistant and are resistant to antibiotics such as the macrolides and aminoglycosides, even though the mechanisms of action of these antibiotics are different than that of the betalactams. MRSA became prevalent by the late 1970s, but MRSA infections usually were confined to the large hospital setting. Community-acquired methicillinresistant S. aureus (CA-MRSA) infections were very unusual, particularly in children, until the 1990s, when CA-MRSA emerged in the United States. Chicago Children’s Hospital reported that the number of children hospitalized with CA-MRSA increased from 8
INTRODUCTION
The emergence of antimicrobial resistance among a number of bacterial pathogens changes the way we practice medicine and places some of our patients at risk of dying from their infections. The overuse and misuse of antibiotics are major contributing factors to bacterial resistance; therefore it is incumbent on each of us to use antibiotics appropriately. This article reviews some of the clinical problems we face as a result of bacterial resistance and then discusses potential solutions, with an emphasis on approMiller Children’s Hospital, Long Beach, CA; and University of California, Irvine, CA. Key words: Bacterial resistance, quinupristin/dalfopristin, linezolid, fluoroquinolones. Address for reprints: Jay M. Lieberman, M.D., Miller Children’s Hospital, 2801 Atlantic Avenue, P.O. Box 1428, Long Beach, CA 90801-1428. Fax 562-997-9634; E-mail [email protected].
1143
1144
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
in the 3-year period from 1988 to 1990 to 35 in the 3-year period from 1993 to 1995.3 In south Texas, 53 CA-MRSA infections were identified between 1997 and 2000, compared with just 7 cases between 1990 and 1996.4 The proportion of community-acquired S. aureus infections in children hospitalized at Texas Children’s Hospital in Houston that was methicillinresistant increased from 35% in February 2000 to 67% in January 2002.5 In 1999 the CDC reported 4 pediatric deaths from CA-MRSA in Minnesota and North Dakota.6 The emergence of CA-MRSA as a significant pediatric pathogen in many parts of the US has important clinical implications. Physicians need to know the prevalence of CA-MRSA in their communities and, in areas where CA-MRSA is prevalent, children hospitalized with potentially life-threatening staphylococcal infections, such as endocarditis, should be empirically treated with vancomycin until susceptibilities are available. For non-life-threatening infections, such as lymphadenitis, cellulitis, osteomyelitis or pneumonia in nontoxic patients, clindamycin is usually an appropriate choice.7 Community-acquired MRSA are much more likely to be susceptible to clindamycin than are hospital-acquired MRSA.2– 4 To further complicate matters for clinicians, MRSA that are clindamycin-susceptible but erythromycinresistant may exhibit inducible resistance to clindamycin (i.e. on exposure to clindamycin, such isolates may develop resistance to clindamycin). At the University of Illinois in Chicago, 33 of 88 clindamycin-susceptible MRSA isolates were erythromycin-resistant.8 Evaluation for inducible clindamycin resistance using the “D test” showed that 31 of the 33 isolates exhibited inducible resistance. There was one clinical failure caused by such an isolate; a 9-month-old boy with empyema caused by a clindamycin-susceptible, erythromycinresistant MRSA developed a clindamycin-resistant isolate during clindamycin therapy. Therefore clindamycin should not be prescribed for long term therapy of significant MRSA infections, such as osteomyelitis or empyema, unless the organism is documented to lack inducible resistance to clindamycin. In contrast to the report from Chicago,8 the prevalence of MRSA with inducible clindamycin resistance appears to be lower in other geographic regions.7 Penicillin-resistant Streptococcus pneumoniae. Clinical isolates of S. pneumoniae are reported as susceptible (MIC ⱕ 0.06 g/ml), intermediate (0.12 g/ml ⱕ MIC ⱕ 1 g/ml), or resistant (sometimes referred to as highly resistant; MIC ⱖ 2 g/ml) to penicillin. The clinical significance of these breakpoints is that infections caused by intermediate strains of pneumococcus, with the exception of meningitis, are likely to respond to third generation cephalosporins or even high dose penicillin. Commonly used beta-lactam
Vol. 22, No. 12, Dec. 2003
antibiotics therefore will often be effective for pneumonia, otitis media or sinusitis caused by an intermediate strain of pneumococcus. On the other hand if the pneumococcus is highly resistant, penicillin will not be effective, and these organisms may also be resistant to cefotaxime and ceftriaxone. Penicillin-resistant pneumococci, like CA-MRSA, emerged in the US in the 1990s. In a study of invasive pneumococcal isolates from eight sites around the US in 1998, 24% were nonsusceptible (either intermediate or highly resistant) and 14% overall were highly resistant.9 Similarly a national surveillance study performed in 1999 through 2000 showed that 34% of clinical isolates (invasive and noninvasive) were penicillin-nonsusceptible and 22% overall were highly resistant.10 Resistance had increased markedly compared with a similar study from 1994 through 1995 when 24% of isolates were nonsusceptible and 10% overall were highly resistant.10 As with CA-MRSA the emergence of drug-resistant pneumococci has changed pediatric practice. A child who is hospitalized with a potentially life-threatening pneumococcal infection, such as definite or probable bacterial meningitis, should be treated with an empiric antibiotic regimen that includes vancomycin in addition to cefotaxime or ceftriaxone.11 Importantly vancomycin is not indicated for all children hospitalized with possible or probable pneumococcal infections, such as pneumonia, unless they are critically ill. The treatment for documented resistant invasive pneumococcal infections, such as meningitis, should be based on susceptibility results and may require vancomycin plus another agent such as ceftriaxone or cefotaxime, meropenem and/or rifampin. Some fluoroquinolone antibiotics (e.g. moxifloxacin, gatifloxacin) have excellent activity against penicillin-resistant pneumococci and, although these agents are not yet approved for use in children ⬍18 years of age, they may have a role in the management of serious, resistant pneumococcal infections in children. Consultation with an infectious disease specialist should be strongly considered to assist in the management of invasive pneumococcal infections caused by nonsusceptible organisms. For the more common pneumococcal infections, such as acute otitis media and sinusitis, therapy can be problematic because no oral agent is active against all resistant strains. A consensus statement on otitis media by a CDC working group and clinical practice guidelines for sinusitis from the American Academy of Pediatrics (AAP) provide some recommendations for the management of these infections in an era of pneumococcal resistance.12, 13 Amoxicillin is the drug of choice for uncomplicated acute otitis media or sinusitis regardless of the local prevalence of resistant pneumococci. Even when pneumococci are resistant to penicillin, sufficient concentrations of amoxicillin can often be
Vol. 22, No. 12, Dec. 2003
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
achieved in middle ear and sinus fluid to successfully treat the infection. For children with ear infections who are at increased risk of having a resistant pneumococcal infection (i.e. young infants and those who have recently received antibiotics or who attend day care), high dose amoxicillin (80 to 90 mg/kg/day) is recommended, and many experts recommend high dose amoxicillin for all children with acute otitis media. For children with otitis media who do not respond clinically after 2 to 3 days of amoxicillin therapy, several drugs may be useful as secondary agents, including high dose amoxicillin/clavulanate, cefdinir, cefuroxime axetil, cefpodoxime proxetil or a single intramuscular dose of ceftriaxone. Some data, however, suggest that three once daily doses of ceftriaxone may be required for penicillin-nonsusceptible pneumococcal ear infections.14 It is important to emphasize that some antibiotics commonly used to treat children with ear and sinus infections are unlikely to be effective against nonsusceptible strains of pneumococcus.12 Cefaclor, loracarbef and cefixime, for example, are poorly active against these organisms and therefore should not be used as first line therapy for acute otitis media or sinusitis. It might be thought that other oral antibiotics, such as trimethoprim-sulfamethoxazole and the macrolides, would maintain their activity against penicillinresistant pneumococci because they have a mechanism of action different from that of penicillin. However, as with MRSA, penicillin-resistant pneumococci are usually multidrug-resistant. More than 80% of penicillinresistant pneumococci are also resistant to trimethoprim-sulfamethoxazole and more than one-half are resistant to the macrolides.9 Vancomycin-resistant Enterococcus. Enterococci are normal inhabitants of the human gastrointestinal tract. These bacteria, which are intrinsically resistant to most antimicrobials, including cephalosporins, generally do not cause significant infections in otherwise healthy children. However, enterococci are common causes of hospital-acquired infection, in large part because the widespread use of cephalosporins in hospitalized patients kills most Gram-negative enteric bacteria and leaves enterococci as the predominant organism.15 Therapy of enterococcal infections has become increasingly problematic because of the emergence of resistance. Before 1983 all strains were susceptible to ampicillin, and the recommended therapy for serious enterococcal infections was a synergistic combination of ampicillin and gentamicin. With the emergence of ampicillin resistance, vancomycin became the drug of choice for serious ampicillin-resistant enterococcal infections. In 1986, however, vancomycin-resistant enterococci (VRE) were first reported,16 and rates of isolation of VRE in hospitals increased steadily
1145
through the 1990s.17 From the clinical perspective the emergence of VRE was important because these isolates were often resistant to all available antibiotics, meaning that some patients had untreatable bacterial infections. Vancomycin resistance among enterococci is also important because it is plasmid-mediated. The capacity for vancomycin resistance, therefore, could be transferred in the laboratory to other Gram-positive bacteria. The major concern was the clinical consequence when S. aureus or Streptococcus pneumoniae became vancomycin-resistant. Vancomycin-resistant Staphylococcus aureus. Clinical isolates of MRSA that were intermediate to vancomycin, called vancomycin-intermediate S. aureus (VISA), were first identified in patients in Japan in 199618; as of June 2002, 8 VISA infections had been documented in patients in the US.19 The mechanism of vancomycin resistance among VISA is not the same as it is for VRE. In June 2002 the first clinical isolate of vancomycinresistant S. aureus (VRSA) was reported from a patient in Michigan.19 The patient was a 40-year-old woman with multiple medical problems, including diabetes mellitus, peripheral vascular disease and chronic renal failure. She had recurrent infections of foot ulcers and received multiple courses of broad spectrum antibiotics to treat these infections. In April 2002 the patient developed MRSA bacteremia and was treated with vancomycin. In June 2002 cultures from a suspected catheter exit site infection grew VRSA that contained the vanA gene that confers vancomycin resistance on VRE. A second documented VRSA infection was reported from Pennsylvania in September 2002. This patient also had chronic foot ulcers, and the VRSA isolate contained the vanA resistance gene.20 For these two patients with VRSA infection, there were other therapeutic options, but the threat of untreatable S. aureus infections looms closer on the horizon. It seems only a matter of time before children develop common infections, such as staphylococcal cellulitis or lymphadenitis, that are resistant to all routinely used oral antibiotics. Why bacterial resistance? Microbes have genetic plasticity, which means that they have the capacity to evolve in response to their environment. The major impetus for developing resistance is selective pressure resulting from antibiotic use. The bacteria that survive are those that develop mechanisms to avoid being killed by antibiotics. What is this antibiotic pressure? In the United States, an estimated 126 million courses of antibiotics were prescribed in the ambulatory setting in 2000.21 Pediatricians have a special responsibility for controlling this problem because children account for a disproportionate share of the antibiotics used. Ear infec-
1146
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
tions alone resulted in almost 30 million office visits in 1997. With all this selective pressure from antibiotic use, bacterial resistance emerges. Because of bacterial resistance, patients present with more serious infections or with infections that are more difficult to treat. This leads to more antibiotic use and the use of more broad spectrum agents. And so a vicious cycle develops. For example it is necessary to limit vancomycin use because of VRE and concerns about the emergence of vancomycin resistance among staphylococci and streptococci. However, because of the increasing prevalence of MRSA and drug-resistant pneumococci, we use more vancomycin. The place to break this vicious cycle is to decrease antibiotic use and thereby decrease the pressure on bacteria to develop resistance. Three major approaches are advocated to combat bacterial resistance: (1) develop new antibiotics to treat resistant organisms; (2) vaccinate to prevent infections; and (3) improve our use of antibiotics. NEW ANTIBIOTICS
Quinupristin/dalfopristin. Quinupristin/dalfopristin (Synercid) is a semisynthetic antibiotic that combines two streptogramin compounds and is the first licensed antibiotic in its class.22 It inhibits bacterial protein synthesis and is available only as an intravenous product. Its spectrum of activity is similar to that of vancomycin, with excellent activity against Grampositive pathogens, including many resistant strains. Quinupristin/dalfopristin is active against staphylococci, including MRSA, pneumococci, including penicillin-resistant strains, and Enterococcus faecium, including VRE (but not Enterococcus faecalis). Its major value is that it provides a therapeutic option for infections caused by vancomycin-resistant E. faecium, VISA or VRSA. In addition quinupristin/dalfopristin may be useful for treatment of serious Gram-positive infections in patients who are allergic to, or intolerant of, beta-lactams and vancomycin. Unfortunately there are already reports of VRE and MRSA resistant to quinupristin/dalfopristin since its licensure in 1999.23, 24 Linezolid. Linezolid (Zyvox) is the first licensed oxazolidinone antibiotic.25 The oxazolidinones, synthetic compounds unrelated to other antimicrobials, inhibit bacterial protein synthesis. Linezolid has limited activity against selected Gram-negatives and anaerobes but is highly active against Gram-positive bacteria, including resistant strains. Like quinupristin/dalfopristin, linezolid is active against MRSA, penicillin-resistant pneumococci and vancomycin-resistant E. faecium. Unlike quinupristin/dalfopristin, linezolid also is active against E. faecalis. Linezolid is available in both intravenous and oral preparations and is 100% bioavailable after oral administration. As such it provides an oral therapeutic
Vol. 22, No. 12, Dec. 2003
option for patients with Gram-positive infections resistant to other oral antibiotics. Therapy with linezolid should be limited to patients with infections caused by VRE, VISA or VRSA; for serious Gram-positive infections in patients who cannot tolerate vancomycin or beta-lactam antibiotics; and for patients with resistant Gram-positive infections who have been treated with intravenous vancomycin and can be transitioned to oral therapy. Since linezolid became available in 2000, clinical isolates of VRE and MRSA resistant to linezolid have been reported from treated patients.26 –28 Quinupristin/dalfopristin and linezolid are two valuable additions to our antimicrobial armamentarium, but resistance has already been described. To preserve their value their use should be limited to those rare cases where they are clearly needed. Fluoroquinolones. Although the fluoroquinolones are not new antibiotics, most pediatricians have limited experience with this class of antibiotics. Important features of this drug class include excellent bioavailability after oral administration, achievement of high tissue concentrations and a broad spectrum of activity. In general fluoroquinolones are active against many Gram-positive bacteria (the “newer” quinolones, moxifloxacin and gatifloxacin, are particularly active against Streptococcus pneumoniae) and many Gramnegative bacteria. Some quinolones (ciprofloxacin being the most potent) have significant activity against Pseudomonas aeruginosa.29 The quinolones are therefore attractive agents to use for treatment of selected children with serious bacterial infections. The quinolones have a unique mechanism of action; they inhibit two bacterial enzymes, DNA gyrase and topoisomerase IV, that are essential for bacterial DNA synthesis. Because they target bacterial sites distinct from the site of action of other antibiotics, it was hypothesized by some that resistance might be less likely to occur or slower to develop.30 Unfortunately these hopes were not borne out. Oral ciprofloxacin first became available in the US in October 1987 and rapidly became a widely prescribed antibiotic. By 1989 it was the fourth most prescribed antibiotic in the country, with ⬎5 million prescriptions filled.31 During the last decade a number of other fluoroquinolones have become available, including ofloxacin, levofloxacin, moxifloxacin and gatifloxacin. With widespread use during the past 15 years, quinolone resistance has emerged among a number of bacteria. Four such organisms are highlighted here. Neisseria gonorrhoeae. Fluoroquinolone antibiotics, such as ciprofloxacin, ofloxacin and levofloxacin, given as a single oral dose are among the recommended therapies for uncomplicated gonorrhea. However, N. gonorrhoeae isolates resistant to the quinolones emerged in the 1990s and are now prevalent in parts of Asia and the Pacific. Such isolates have been identified
Vol. 22, No. 12, Dec. 2003
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
only sporadically throughout the US, although in Hawaii the percentage of isolates that are ciprofloxacinresistant increased from 1.4% in 1997 to 14.3% in 2000.32, 33 As a result, before treating a patient with gonorrhea, a travel history should be obtained from both the patient and their sexual partner(s). If either is likely to have acquired the infection in Asia, the Pacific Islands or Hawaii, then a quinolone should not be used. Because of an increased prevalence of quinolone resistance among N. gonorrhoeae isolates in California, the CDC has also stated that the use of fluoroquinolones in that state “is probably inadvisable.”33 S. pneumoniae. The newer quinolones (e.g. moxifloxacin, gatifloxacin) are now among the recommended agents for the empiric treatment of community-acquired pneumonia in adults. 34 In Canada prescriptions for quinolones in general increased almost 7-fold between 1988 and 1998 (from 0.8 to 5.5 prescriptions per 100 persons per year).35 Through 1993 pneumococci with reduced susceptibility to the quinolones had not been identified but, by 1997 through 1998, the prevalence of S. pneumoniae strains nonsusceptible to ciprofloxacin isolated from Canadian adult patients had increased to 2.9%. All strains isolated from children were susceptible. Furthermore patients with pneumococcal pneumonia who failed empiric levofloxacin therapy because of infections with levofloxacin-resistant strains (including patients whose isolates developed resistance during therapy) have been reported.36, 37 Although the overall prevalence of quinolone-resistant pneumococci remains relatively low, it is interesting to recognize that penicillin was available for almost 50 years before clinically significant penicillin resistance emerged. It took fewer than 10 years for quinolone resistance to develop among the pneumococci. Campylobacter/Salmonella. The quinolones are widely prescribed for the treatment of patients with bacterial gastroenteritis because this class of drugs is active against a broad range of bacterial pathogens that cause diarrhea, including Salmonella, Shigella, Campylobacter and Yersinia. In Minnesota, however, the proportion of Campylobacter jejuni resistant to the quinolones increased from 1.3% in 1992 to 10.2% in 1998.38 Many of these cases were associated with foreign travel and recent quinolone use. This phenomenon is not limited to Minnesota; 40.5% of C. jejuni isolates were fluoroquinolone-resistant in one Pennsylvania health care system in 2001.39 Fluoroquinolone resistance also has emerged among Salmonella species. In Taiwan, ciprofloxacin resistance was not seen among Salmonella enterica serotype choleraesuis until 2000. By the third quarter of 2001, 60% of isolates in Taiwan were ciprofloxacin-resistant.40 An analysis of S. enterica isolates from Finnish travelers also showed that the proportion with reduced suscep-
1147
tibility to ciprofloxacin increased from 3.9% in 1995 to 23.5% in 1999.41 One reason quinolone resistance has emerged among enteric bacteria is that, in some regions of the world, these antibiotics are used in livestock and poultry not only to treat infections in the animals but, more importantly, to promote growth after administration of subtherapeutic concentrations.42 This long term exposure to low levels of antibiotics provides an ideal environment for the selection of resistant bacteria in the animals. Although quinolones are not approved for growth promotion, they are known to be misused, especially outside the US.43 In the US quinolone antibiotics were approved for therapeutic use in poultry in 1995. In Minnesota C. jejuni was isolated from 74% of 91 retail chicken products in 1997, and 14% of these isolates were ciprofloxacin-resistant.38 Many public health experts want to prohibit the use of antibiotics in poultry, especially those antibiotics that are used to treat infections in humans.44 In 1999 the European Union banned the use of four such antibiotics as growth promoters.45 The US Food and Drug Administration may soon follow suit. The experience with the quinolones exemplifies the lesson that inappropriate use of an antibiotic hastens the development of resistance. The more an antibiotic is used, the more pressure there is on bacteria to develop resistance. If antibiotics are not used judiciously, they can lose their value and thus not be available for patients who really need them. Appropriate use of fluoroquinolones in children. Although the quinolones are not currently approved for use in patients younger than 18 years of age, they already have an established role in certain high risk pediatric populations. They are commonly used to treat pulmonary exacerbations caused by P. aeruginosa in children who have cystic fibrosis and may also have a role in the prevention or treatment of infections in children with cancer. Several potentially appropriate uses for quinolones in otherwise healthy children are listed in Table 1.
TABLE 1. Possible uses for fluoroquinolone antibiotics in otherwise healthy children* Infections caused by Pseudomonas aeruginosa or other multidrug-resistant Gram-negative bacteria Urinary tract infection Chronic suppurative otitis media or malignant otitis externa Chronic osteomyelitis Complicated middle ear and mastoid infections Bacterial gastroenteritis caused by a multidrug-resistant organism, e.g. Shigella Typhoid fever Mycobacterial infections Anthrax prophylaxis or treatment * Fluoroquinolone antibiotics are not licensed for use in individuals younger than 18 years of age, except in the case of anthrax treatment. If use is recommended for a patient younger than 18 years of age, the risks and benefits should be explained to the patient, when appropriate, and parents.
1148
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
They should not be used to treat children with colds or bronchitis or for children who have infections susceptible to other oral antibiotics. In general the quinolones should be reserved for treating specific bacterial infections (e.g. P. aeruginosa) that are resistant to commonly used antibiotics or when the use of an oral quinolone allows outpatient management of a serious infection for which no other oral agent is available. IMMUNIZATIONS
New antibiotics will never completely solve the bacterial resistance problem because organisms eventually develop resistance. New vaccines, on the other hand, may provide a solution. By the 1970s a significant proportion of Haemophilus influenzae type b (Hib) isolates was resistant to ampicillin and chloramphenicol. It seemed inevitable that Hib would develop resistance to ceftriaxone and cefotaxime. However, antibiotic-resistant Hib meningitis is no longer of concern because widespread use of the Hib conjugate vaccines has eliminated the disease. Similarly concerns about treating resistant pneumococcal infections can be alleviated through use of the pneumococcal conjugate vaccine. Vaccination against viral diseases also can reduce antibiotic use. Preventing chickenpox through use of the varicella vaccine can avert secondary bacterial infections caused by S. aureus and eliminate concerns about possible MRSA infection. Preventing influenza may thwart secondary bacterial ear infections and pneumonia. In a study of a nasal spray influenza vaccine in children, vaccinated children had 21% fewer febrile illnesses and 30% fewer episodes of febrile otitis media than did unvaccinated controls.46 Widespread vaccination against influenza among young children, as encouraged by the current recommendations,47 will lead to fewer fevers and fewer antibiotic prescriptions. Decreasing antibiotic use can reduce the emergence of resistance. IMPROVING ANTIBIOTIC USE
Judicious antibiotic use means that antibiotics are prescribed only when indicated and that the drug chosen is the most narrow spectrum agent that will be effective. Appropriate use means choosing not only the correct antibiotic but also the appropriate dose and duration, factors that can influence the development and carriage of resistant organisms.29, 48 In an observational study of children in France, the use of an oral beta-lactam agent was associated with an increased risk of pharyngeal carriage of penicillinresistant Streptococcus pneumoniae. The risk was highest in those children who had been prescribed a lower than recommended dose of the antibiotic and in those who had received ⬎5 days of therapy.49 A randomized trial conducted in Chile confirmed these find-
Vol. 22, No. 12, Dec. 2003
ings. The rate of carriage of penicillin-nonsusceptible pneumococci was significantly lower in children prescribed amoxicillin at 90 mg/kg/day for 5 days compared with children prescribed 40 mg/kg/day for 10 days.50 Understanding that low dose and/or prolonged antibiotic usage selects for bacterial resistance can lead to beneficial changes in physicians’ antibiotic prescribing practices.51 The results of a metaanalysis suggest that 5 days of antibiotic therapy is effective for uncomplicated acute otitis media,52 and short course therapy is recommended for children 2 years of age and older with uncomplicated ear infections.11 Clinical research may define other pediatric infections for which a shorter course of antibiotics is appropriate. The importance of appropriate antibiotic use is magnified by the fact that these drugs have an impact on the community as well as on the child for whom they are prescribed. An antibiotic alters a child’s microbial flora and, for example, increases the likelihood that the child will be colonized with a penicillin-resistant pneumococcus. Although that child may never develop pneumococcal disease, children in the same day-care center or a younger sibling may acquire that resistant organism and develop an ear infection or meningitis. After an 11-month-old child in a Georgia day-care center developed refractory otitis media caused by a multidrug-resistant pneumococcus, other children in the center were evaluated for nasal carriage of the organism. Of 21 children tested 10 (48%) carried the same highly resistant pneumococcus.53 Similarly a child in an intensive care unit who is treated with extended spectrum cephalosporins may become colonized with resistant pathogens such as VRE or multidrug-resistant Gram-negative bacteria. These highly resistant pathogens can then be transmitted via the hands of a health care worker to a child in a neighboring bed who may develop a serious infection. The implication is that every time an antibiotic is prescribed, there is a multiplier effect. Every antibiotic given to a child may adversely affect 2 or 5 or 10 children. However, this fact also empowers prescribers, because it means that for every antibiotic not prescribed, 2 or 5 or 10 children are protected from the potential adverse consequences. The good news is that bacterial resistance is to some degree reversible. In response to an increase in erythromycin resistance among group A streptococci in Finland, nationwide recommendations were issued to reduce the use of macrolide antibiotics. As a result macrolide consumption declined by ⬃40%, and the frequency of erythromycin resistance among group A streptococcal isolates subsequently declined by almost one-half.54 Reducing antibiotic use should be effective, because resistant bacteria have no competitive advantage in
Vol. 22, No. 12, Dec. 2003
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
the absence of antibiotic exposure and because colonization with resistant pathogens is usually transient. A study of nasopharyngeal carriage of penicillinresistant pneumococci revealed that cultures were negative within 4 weeks in 68% of carriers, within 8 weeks in 87% and within 12 weeks in 94%.55 Because carriage of these resistant bacteria resolves spontaneously, susceptible strains eventually replace resistant strains in the absence of antibiotic exposure. Antibiotic restrictions do not guarantee that antimicrobial resistance will disappear, however, as demonstrated by a report from the UK.56 Despite a marked decrease in prescriptions for sulfonamides, the frequency of sulfonamide-resistant Escherichia coli did not decrease during an 8-year time period. The reasons for this are not clear, although it may be because the determinants of sulfonamide resistance are genetically linked to other resistance determinants. The AAP and CDC have published principles of judicious antibiotic use for upper respiratory tract infections.57 Key features of these recommendations are highlighted in Table 2. Despite the guidelines inappropriate antibiotic use is common. One report evaluated 531 pediatric office visits in which the discharge diagnosis was cold, upper respiratory tract infection, or bronchitis and found that antibiotics were prescribed for 44% of children with colds, 46% with upper respiratory tract infections and 75% with bronchitis.58 None of these patients required antibiotics, and yet these 3 diagnoses accounted for ⬎20% of all antibiotic prescriptions. In another study physicians were polled regarding
their antibiotic prescribing practices, and 38% of the pediatricians and 58% of the family physicians indicated that they routinely prescribed antibiotics for the common cold.59 In addition 81% of the pediatricians and 93% of the family physicians routinely prescribed antibiotics for bronchitis. A review of their office charts showed that these reported practices correlated with actual practices, given that antibiotics were prescribed for 31% of visits where the common cold was diagnosed. In addition antibiotics were prescribed for 19% of phone encounters and 49% of office visits, including 11% of well-child checkups. There was enormous variability among practitioners, with rates of antibiotic prescribing ranging from 1 to 10 prescriptions per child per year. Pediatricians acknowledge that they sometimes prescribe antibiotics for inappropriate indications60; their reasons for this are multifactorial. Parental pressure is a major factor cited by some clinicians. Parents often desire a tangible product at the conclusion of a visit, and the clinician may feel that they need to satisfy this demand. It is clear that any educational campaign to reduce inappropriate antibiotic use in children must target parents as well as clinicians. Other factors that can influence prescribing practices include concerns about legal liability, economic pressures to evaluate and examine patients quickly and incorrect perceptions about the effectiveness of antibiotics for certain infections.60, 61 Changing physician (and parental) behavior is complex and will require a multifaceted approach, but there is some evidence to suggest this can be accom-
TABLE 2. Principles of judicious use of antimicrobial agents for upper respiratory tract infections* Disease
Principles
Otitis media
1. Antimicrobials are indicated for the treatment of AOM, but the diagnosis requires documented middle ear effusion and signs or symptoms of acute local or systemic illness. 2. A narrow spectrum antibiotic (e.g. amoxicillin) should be used for initial episodes of AOM. 3. Antimicrobials are not indicated for initial treatment of otitis media with effusion, although treatment may be indicated if effusions persist for ⱖ3 mo. 4. Antimicrobial prophylaxis should be reserved for control of recurrent AOM, defined as ⱖ3 distinct and well-documented episodes in 6 mo or ⱖ4 episodes in 12 mo.
Acute sinusitis
1. Clinical diagnosis of bacterial sinusitis requires: nasal discharge and daytime cough without improvement for 10 to 14 days; or more severe signs and symptoms (i.e. fever ⱖ39°C, facial swelling, facial pain). 2. Initial antimicrobial treatment of acute sinusitis should be with the most narrow spectrum agent that is active against the likely pathogens.
Cough illness/bronchitis
1. Nonspecific cough illness/bronchitis in children, regardless of duration, does not warrant antimicrobial treatment.
Pharyngitis
1. Diagnosis of group A streptococcal pharyngitis should be made based on results of appropriate laboratory tests in conjunction with clinical and epidemiologic findings. 2. Antimicrobial therapy should not be given to a child with pharyngitis in the absence of documented group A streptococcal infection. Other rare causes of bacterial pharyngitis, e.g. diphtheria, may require therapy. 3. Penicillin remains the drug of choice for treating group A streptococcal pharyngitis.
Common cold
1. Antimicrobial agents should not be given for the common cold. 2. Mucopurulent rhinitis (thick, opaque or discolored nasal discharge) frequently accompanies the common cold and is not an indication for antimicrobial treatment unless it persists for 10 –14 days suggesting possible sinusitis.
* Adapted from Reference 57, with permission.
1149
1150
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
plished. One study evaluated an educational intervention for pediatricians and family physicians.62 Principles of judicious antibiotic use were discussed with the physicians twice over a 4-month period, and parents were mailed a brochure on antibiotic use. Antibiotic prescribing practices before and after the intervention were compared, as they were in “control” practices in which no intervention was done. In children 3 to 36 months of age, antibiotic dispensing decreased 18.6% in the intervention group vs. 11.4% in the control practices. In another study a community-based intervention trial targeted parents and pediatric primary care providers for education regarding judicious antibiotic use.63 The median number of prescriptions for liquid antibiotics per clinician declined 11% in the intervention region, whereas it increased 12% in the control region. The median number of solid antibiotic prescriptions (tablets and capsules) declined by 19% and 8% in the intervention and control regions, respectively. The results of these two studies should be interpreted with some caution because of baseline differences in antibiotic prescribing rates between the intervention and control groups. Nonetheless they support the idea that educating physicians and parents can positively impact antibiotic use. It is interesting that antibiotic use decreased not only in the intervention groups and regions, but also in many of the control practices and regions. This is a nationwide trend. From 1989 to 1990 through 1999 to 2000, overall antibiotic prescription rates (per patient visit) by office-based physicians in the US declined by 29% for children younger than 15 years of age.64 For children younger than 5 years, the group with the highest antibiotic use, antibiotic prescribing dropped by 41% between 1995 and 1999.65 The message that we need to improve our antibiotic prescribing seems to have been heard. Each of us must do what we can to ensure that this trend continues, because our reward will be less bacterial resistance and healthier children. CONCLUSIONS
Bacterial resistance threatens our ability to treat both common and serious infections in children. Although new antibiotics can effectively treat some resistant pathogens and more research is needed to develop novel antimicrobials, bacteria will eventually develop resistance to any antibiotic with time. The misuse and overuse of antibiotics drive the emergence and spread of resistance. Eliminating inappropriate antibiotic use and promoting more judicious use are essential parts of the solution. REFERENCES 1. Neu HC. The crisis in antibiotic resistance. Science 1992;257: 1064 –73. 2. Chambers HF. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis 2001;7:178 – 82.
Vol. 22, No. 12, Dec. 2003
3. Herold BC, Immergluck LC, Maranan MC, et al. Communityacquired methicillin-resistant Staphylococcus aureus infections in children with no predisposing risk. JAMA 1998;279: 593– 8. 4. Fergie JE, Purcell K. Community-acquired methicillinresistant Staphylococcus aureus infections in south Texas children. Pediatr Infect Dis J 2001;20:860 –3. 5. Sattler CA, Mason EO Jr, Kaplan SL. Prospective comparison of risk factors and demographic and clinical characteristics of community-acquired, methicillin-resistant versus methicillin-susceptible Staphylococcus aureus infection in children. Pediatr Infect Dis J 2002;21:910 –7. 6. Centers for Disease Control and Prevention. Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus: Minnesota and North Dakota, 1997– 1999. MMWR 1999;48:707–10. 7. Martinez-Aguilar G, Hammerman W, Mason EO Jr, Kaplan SL. Clindamycin treatment of invasive infections caused by community-acquired, methicillin-resistant and methicillinsusceptible Staphylococcus aureus in children. Pediatr Infect Dis J 2003;22:593– 8. 8. Frank AL, Marcinak JF, Mangat PD, et al. Clindamycin treatment of methicillin-resistant Staphylococcus aureus infections in children. Pediatr Infect Dis J 2002;21:530 – 4. 9. Whitney CG, Farley MM, Hadler J, et al. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med 2000;343:1917–24. 10. Doern GV, Heilmann KP, Huynh HK, Rhomberg PR, Coffman SL, Brueggemann AB. Antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in the United States during 1999 –2000, including a comparison of resistance rates since 1994 –1995. Antimicrob Agents Chemother 2001;45:1721–9. 11. American Academy of Pediatrics. Pneumococcal infections. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003:490 –500. 12. Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance: a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working Group. Pediatr Infect Dis 1999;18:1–9. 13. American Academy of Pediatrics, Subcommittee on management of sinusitis and committee on quality improvement. Clinical practice guideline: management of sinusitis. Pediatrics 2001;108:798 – 808. 14. Leibovitz E, Piglansky L, Raiz S, Press J, Leiberman A, Dagan R. Bacteriologic and clinical efficacy of one day vs. three day intramuscular ceftriaxone for treatment of nonresponsive acute otitis media in children. Pediatr Infect Dis J 2000;19:1040 –5. 15. Rice LB. Emergence of vancomycin-resistant enterococci. Emerg Infect Dis 2001;7:183–7. 16. Uttley AH, Collins CH, Naidoo J, George RC. Vancomycinresistant enterococci. Lancet 1988;1:57– 8. 17. Murray BE. Vancomycin-resistant enterococcal infections. N Engl J Med 2000;342:710 –21. 18. Smith TL, Pearson ML, Wilcox KR, et al. Emergence of vancomycin resistance in Staphylococcus aureus. N Engl J Med 1999;340:493–501. 19. Chang S, Sievert DM, Hageman JC, et al. Infection with vancomycin-resistant Staphylococcus aureus containing the vanA resistance gene. N Engl J Med 2003;348:1342–7. 20. Centers for Disease Control and Prevention. Vancomycinresistant Staphylococcus aureus: Pennsylvania, 2002. MMWR 2002;51:902. 21. McCaig LF, Besser RE, Hughes JM. Antimicrobial drug prescriptions in ambulatory care settings, United States, 1992–2000. Emerg Infect Dis 2003;9:432–7. 22. Harrison CJ. Quinupristin/dalfopristin. Semin Pediatr Infect Dis 2001;12:200 –10. 23. Dowzicky M, Talbot GH, Feger C, Prokocimer P, Etienne J, Leclercq R. Characterization of isolates associated with emerging resistance to quinupristin/dalfopristin (Synercid®)
Vol. 22, No. 12, Dec. 2003
24.
25. 26. 27. 28.
29. 30. 31. 32.
33. 34.
35.
36. 37.
38. 39. 40. 41.
42. 43.
44.
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
during a worldwide clinical program. Diagn Microb Infect Dis 2000;37:57– 62. Rose CM, Reilly KJ, Haith LR, et al. Emergence of resistance of vancomycin-resistant Enterococcus faecium in a thermal injury patient treated with quinupristin-dalfopristin and cultured epithelial autografts for wound closure. Burns 2002; 28:696 – 8. Diekema DJ, Jones RN. Oxazolidinone antibiotics. Lancet 2001;358:1975– 82. Herrero IA, Issa NC, Patel R. Nosocomial spread of linezolidresistant, vancomycin-resistant Enterococcus faecium. N Engl J Med 2002;346:867–9. Tsiodras S, Gold HS, Sakoulas G, et al. Linezolid resistance in a clinical isolate of Staphylococcus aureus. Lancet 2001; 358:207– 8. Pai MP, Rodvold KA, Schreckenberger PC, Gonzales RD, Petrolatti JM, Quinn JP. Risk factors associated with the development of infection with linezolid- and vancomycinresistant Enterococcus faecium. Clin Infect Dis 2002;35: 1269 –72. Scheld WM. Maintaining fluoroquinolone class efficacy: review of influencing factors. Emerg Infect Dis 2003;9:1–9. Kayser FH. The quinolones: mode of action and mechanism of resistance. Res Clinic Forums 1985;7:17–27. Frieden TR, Mangi RJ. Inappropriate use of oral ciprofloxacin. JAMA 1990;264:1438 – 40. Centers for Disease Control and Prevention. Fluoroquinolone-resistance in Neisseria gonorrhoeae, Hawaii, 1999, and decreased susceptibility to azithromycin in N. gonorrhoeae, Missouri, 1999. MMWR 2000;49:833–7. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines. MMWR 2002;51(RR6):36 – 42. Bartlett JG, Dowell SF, Mandell LA, File TM Jr, Musher DM, Fine MJ. Practice guidelines for the management of community-acquired pneumonia in adults. Clin Infect Dis 2000;31: 347– 82. Chen DK, McGeer A, de Azavedo JC, Low DE. Decreased susceptibility of Streptococcus pneumoniae to fluoroquinolones in Canada: Canadian Bacterial Surveillance Network. N Engl J Med 1999;341:233–9. Davidson R, Cavalcanti R, Brunton JL, et al. Resistance to levofloxacin and failure of treatment of pneumococcal pneumonia. N Engl J Med 2002;346:747–50. Kays MB, Smith DW, Wack ME, Denys GA. Levofloxacin treatment failure in a patient with fluoroquinolone-resistant Streptococcus pneumoniae pneumonia. Pharmacotherapy 2002;22:395–9. Smith KE, Besser JM, Hedberg CW, et al. Quinoloneresistant Campylobacter jejuni infections in Minnesota, 1992–1998. N Engl J Med 1999;340:1525–32. Nachamkin I, Ung H, Li M. Increasing fluoroquinolone resistance in Campylobacter jejuni, Pennsylvania, USA, 1982– 2001. Emerg Infect Dis 2002;8:1501–3. Chiu CH, Wu TL, Su LH, et al. The emergence in Taiwan of fluoroquinolone resistance in Salmonella enterica serotype choleraesuis. N Engl J Med 2002;346:413–9. Hakanen A, Koitlainen P, Huovinen P, Helenius H, Siitonen A. Reduced fluoroquinolone susceptibility in Salmonella enterica serotypes in travelers returning from Southeast Asia. Emerg Infect Dis 2001;7:996 –1003. Tollefson L, Miller MA. Antibiotic use in food animals: controlling the human health impact. J AOAC Int 2000;83: 245–54. Velazquez JB, Jimenez A, Chomon B, Villa TG. Incidence and transmission of antibiotic resistance in Campylobacter jejuni and Campylobacter coli. J Antimicrob Chemother 1995;35: 173– 8. Center for Science in the Public Interest. Protecting the crown jewels of medicine: a strategic plan to preserve the effectiveness of antibiotics. Washington, DC, 1998. [Center for Science in the Public Interest web site]. Available at http://www.cspinet.org/reports/abiotic.htm. Accessed August 27, 2003.
1151
45. Department of Health and Human Services, Food and Drug Administration. HHS response to House Report 106-157: Agriculture, Rural Development, Food and Drug Administration, and Related Agencies, appropriations bill, 2000. Human-use antibiotics in livestock production. [Center for Veterinary Medicine web site]. Available at http://www.fda.gov/ cvm/antimicrobial/HRESP106_157.htm#execsummary. Accessed August 28, 2003. 46. Belshe RB, Mendelman PM, Treanor J, et al. The efficacy of live attenuated, cold-adapted, trivalent, intranasal influenzavirus vaccine in children. N Engl J Med 1998;338:1405–12. 47. Centers for Disease Control and Prevention. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2003;52 (RR-8):7–10. 48. Craig WA. Does the dose matter? Clin Infect Dis 2001; 33(Suppl 3):S233–7. 49. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of beta-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA 1998; 279:365–70. 50. Schrag SJ, Pen˜ a C, Ferna´ ndez J, et al. Effect of short-course, high-dose amoxicillin therapy on resistant pneumococcal carriage: a randomized trial. JAMA 2001;286:49 –56. 51. Levy SB. Antibiotic resistance: consequences of inaction. Clin Infect Dis 2001;33(Suppl 3):S124 –9. 52. Kozyrskyj AL, Hildes-Ripstein GE, Longstaffe SE, et al. Treatment of acute otitis media with a shortened course of antibiotics: a meta-analysis. JAMA 1998;279:1736 – 42. 53. Centers for Disease Control and Prevention. Multidrugresistant Streptococcus pneumoniae in a child care center: southwest Georgia, December 2000. MMWR 2002;50:1156– 8. 54. Seppala H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. N Engl J Med 1997;337:441– 6. 55. Ekdahl K, Ahlinder I, Hansson HB, et al. Duration of nasopharyngeal carriage of penicillin-resistant Streptococcus pneumoniae: experiences from the South Swedish Pneumococcal Intervention Project. Clin Infect Dis 1997;25:1113–7. 56. Enne VI, Livermore DM, Stephens P, Hall LM. Persistence of sulphonamide resistance in Escherichia coli in the UK despite national prescribing restriction. Lancet 2001;357:1325– 8. 57. American Academy of Pediatrics. Appropriate use of antimicrobial agents. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics, 2003:695–7. 58. Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 1998;279:875–7. 59. Watson RL, Dowell SF, Jayaraman M, Keyserling H, Kolczak M, Schwartz B. Antimicrobial use for pediatric upper respiratory infections: reported practice, actual practice, and parent beliefs. Pediatrics 1999;104:1251–7. 60. Bauchner H, Pelton SI, Klein JO. Parents, physicians, and antibiotic use. Pediatrics 1999;103:395– 401. 61. Avorn J, Solomon DH. Cultural and economic factors that (mis)shape antibiotic use: the nonpharmacologic basis of therapeutics. Ann Intern Med 2000;133:128 –35. 62. Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics 2001;108:1–7. 63. Belongia EA, Sullivan BJ, Chyou PH, Madagame E, Red KD, Schwartz B. A community intervention trial to promote judicious antibiotic use and reduce penicillin-resistant Streptococcus pneumoniae carriage in children. Pediatrics 2001; 108:575– 83. 64. McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA 2002; 287:3096 –102. 65. Halasa NB, Griffin MR, Zhu Y, Edwards KM. Decreased number of antibiotic prescriptions in office-based settings from 1993 to 1999 in children less than five years of age. Pediatr Infect Dis J 2002;21:1023– 8.
Related Documents

Appropriate Antibiotic Use
November 2019 8
Appropriate Technologies
November 2019 23
Appropriate Computing
October 2019 26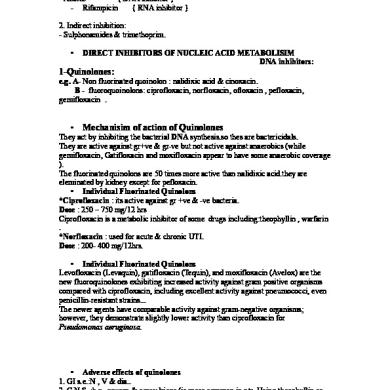
Antibiotic 1
May 2020 13
Antibiotic Policy
April 2020 15